Advantages of
using tracheo-esophageal speech:
- The use of pulmonary air supply for speech
- Natural sounding phonation
- Voice restoration usually occur within 2 weeks of surgery (primary TEP)
- The voice prosthesis may be maintained by patient, increasing independence
Disadvantages:
- Additional surgery is required for secondary puncture
- Daily maintenance of voice prosthesis
- Aspiration may occur if fluids leak through a malfunctioning valve or arround the voice prosthesis
- Dependency on speech and language pathologist
- Cost
Types of voice prosthesis
Voice-prostheses types vary in size, shape, resistance levels, material, insertion techniques and valve life. There are two types of voice prosthesis: an indwelling one that is installed and changed by a speech and language pathologist (SLP) or otolaryngologist and a patient-changed one.
Characteristics of the non-indwelling and indwelling voice prosthesis:
Non-indwelling
- Maintained by patient
- Less expensive
- Tab remains in place
- More frequent replacement
Indwelling
- Managed by health professional
- More expensive
- Tab is optional
- Longer duration in-place
Indication for
voice prosthesis replacement are:
- Leakage through or around the prosthesis
- Poor trachea - esophageal voice
- Ill fitted voice prosthesis – either too long or too short
- Accidental dislodgement
The process of replacing an indwelling voice-prosthesis starts with removal of the old prosthesis; followed by dilation, seizing, and repeated dilation of the puncture; and finally inserting the new prosthesis. The indwelling prosthesis generally lasts a longer time than the patient managed device. However, prosthesis eventually leak mostly because yeast and other microorganisms grow into the silicone leading to incomplete closure of the valve flap. When the valve flap does not close tight anymore, esophageal fluids can pass through the voice prosthesis (see below in Causes of voice prosthesis leak section). Prosthetic options to address leakage through the prosthesis may use biofilm resistant materials, designs that inset the flap into the shaft of the prosthesis to minimize contact with esophageal contents, double valves, and/or magnets.
It is
recommended to test for leakage at least once a week. Testing can be done by
standing in front of a mirror using a flashlight or light directed at the stoma,
taking a drink ( preferably of colored beverage), and look at the prosthesis
while drinking. Coughing is generally induced when leakage occurs.
An indwelling prosthesis can function well for weeks to months. However, some SLPs believe that it should be changed even when it does not leak after six months because, if left for a longer time, it can lead to dilatation of the puncture leading to leakage. ( See picture below)
Vega voice prosthesis after 6 months showing deposits of biofilm that can cause dilation of the puncture fistula)
The patient managed voice prosthesis allows greater degree of independence. It can be changed by the laryngectomee on a regular basis (every 1-2 weeks). Some individuals change the prosthesis only after it starts leaking. The old prosthesis can be cleaned and reused several times.
A number of factors determine an individual's ability to use a patient managed voice prosthesis:
- The location of the puncture should be easily accessible; however, the site of the puncture may, migrate over time, making it less accessible.
- The laryngectomee should have adequate eyesight and good dexterity, enabling him/her to perform the procedure, and capable of following all the steps involved. An indwelling voice prosthesis does not need to be changed as frequently as a patient managed one.
Two videos made by Steve Staton explain how to replace a patient-changed prosthesis: Prosthesis installation 1 and prosthesis installation 2.

A voice prosthesis (Vega TM Atos Medical)
- Poor dexterity
- Poor eye sight
- Poor pulmonary function
- Impaired mental status
- Lack of motivation
- Inability to manage associated care of stoma and voice prosthesis
- Voicing difficulties
- Glosectomy with associated poor articulation
- History of radiation therapy with fibrosis, thereby decreasing the ability of tissue to vibrate
- Esophageal stenosis with stricture
- Extensive surgical resection / reconstruction with involvement of the tongue
- Recurrent aspiration and dislodging of the voice prosthesis
- Difficulty in occluding the stoma
- Proximity of speech pathologist or otolaryngologist
- Lack of support system
- Potential cost and lack of reimbursement
The American Speech - Language - Hearing Association ( ASHA) published guidelines about use of voice prosthesis and HME and their care.
Assessment the
suitability of the patient for tracheoesophageal speech
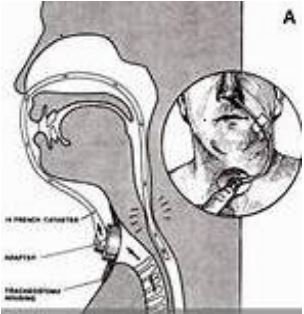
A suffalation test is commonly performed
to assess the suitability of the patient for tracheoesophageal speech and to
guide the selection of an appropriate prosthesis size and type. It involves
passing a catheter through the nose into the esophagus and insufflating
(blowing air) to simulate tracheoesophageal speech. This allows evaluation of
the patient's ability to produce tracheoesophageal voice and assess the
condition of the pharyngoesophageal (PE) segment.
- If the patient can sustain phonation for at least 10 seconds or produce 10-15 syllables per breath during the test, it indicates adequate PE segment integrity for tracheoesophageal speech.
- If the test results are poor, it may indicate issues like hypotonicity, hypertonicity, spasticity, or stricture of the PE segment, which can guide further interventions before prosthesis placement.
- The test helps determine the appropriate prosthesis size and type based on the patient's anatomy and phonatory ability.
However, suffalation testing is not
mandatory in all cases, especially for experienced clinicians who can assess
the suitability for voice prosthesis based on clinical examination and
intraoperative findings. In some cases, the prosthesis may be placed without
prior suffalation testing, and adjustments can be made based on the patient's
postoperative speech outcomes.
Suffalation test
Using a plug allows
continued eating and drinking while waiting for voice prosthesis replacement
due to leaking through. It can be inserted with the non-bristled end of Provox
Brush. (see Picture below) Speaking is not possible with a Plug in place.
Axial CT with contrast, showing TEP in the stomach
Leakage through the voice prosthesis is predominantly due to situations in which the valve can no longer close tightly. This may be due the following: colonization of the valve by a biofilm of fungus; the flap valve may get stuck in the open position; a piece of food, mucus, debris, or hair (in those with a free flap) stuck on the valve (can be addressed by brushing and flushing the prosthesis); development of high pressure in the esophagus when swallowing ( can be addressed by replacing the valve with one with increased resistance such as Activalve or Dual Valve) , or the device coming in contact with the posterior esophageal wall. Leakage is more likely to occur in those who have dentures, are immunocompromised, receive antibiotic or steroid therapies, and during radiation treatment. Inevitably, all prostheses will fail by leaking through, whether from Candida biofilm colonization or simple mechanical failure.
If there is continuing leakage through the prosthesis from the time it is inserted, the problem is generally caused by the flap's valve remaining open because of negative pressure generated by swallowing. Esophageal dysmotility is the main cause for reduced swallow pressure and occurs if the esophageal contractions are not strong enough, are absent, or are not synchronized properly. Low esophageal pressure can even cause the TEP to open inadvertently or close insufficiently during deep inhalation or swallowing leading to leakage. This can be corrected by using a prosthesis that has a greater resistance ( e.g.. Activalve, Dual Valve). Activalve is made of fluroplastic that resists destruction, has magnetic valve closure, and generally last longer. The trade-off is that having such a voice prosthesis may require more effort when speaking. It is nevertheless important to prevent chronic leakage that can lead to aspiration into the lungs.
Granulation around the prosthesis is usually caused by the irritation associated with the presence of prosthesis, especially when it is fitting too tight. It can be removed surgical and the fitness of the prosthesis should be reassessed.
Another cause of leakage around the prosthesis is the presence of narrowing (stricture) of the esophagus. The narrowing of the esophagus forces the laryngectomee to swallow harder, with greater force so that the food/liquid goes through the stricture. Esophageal dilation may help stop the leaking. Other causes of elevated swallow pressure include pharyngo-esophageal spasm, or external compression on the esophagus (e.g., osteophytes). The excess swallowing pressure pushes the food/liquid around the prosthesis.
Several procedures have been used to treat persistent leakage around the prosthesis. These include temporary removal of the prosthesis and replacement with a smaller-diameter catheter to encourage spontaneous shrinkage; using customized prostheses; placing a purse-string suture around the puncture; injection of gel, collagen or micronized AlloDerm® ( LifeCell, Branchburg, N.J. 08876); cauterize with silver nitrate or electrocautery; autologous fat transplantation; inserting a larger prosthesis to stop the leak; allowing the puncture to close after removing the prosthesis or closing it surgically; and performing flap reconstruction followed later by preforming a new puncture.
Increasing the diameter of the prosthesis is generally not recommended. Generally a larger diameter TEP is heavier than a smaller one, and the weakened tissue is often not able to support a bigger device, making the problem even worse.
Some, however, believe that using a larger diameter prosthesis reduces the speaking pressure (larger diameter allows better airflow) which allows greater tissue healing to occur while when the underlying cause (most often reflux) is treated.
The use of a prosthesis using a larger esophageal and/or tracheal flange may be helpful, as the flange acts as a washer to seal the prosthesis against the walls of the esophagus and/or trachea, thus preventing leakage.
The prosthesis may have to be changed if there is an alteration in the quality of the voice especially when the voice becomes weaker or one needs more respiratory effort to speak. This may be due to yeast growth which interferes with the opening of the valve.
- Development of aspiration pneumonia
- Clogging of HME
- Social embarrassment
- Anxiety
- Temporary increase of blood pressure and pulse
- Avoiding food and liquid intake causing dehydration and weight loss
- Emergence of inguinal hernia
- Urinary incontinence ( involuntary leakage of urine)
If the leakage through the voice prosthesis happens within three days after its insertion it may be due to a defective prosthesis or one that was not placed correctly. It takes some time for the yeast to grow. If the prosthesis leaks when new, it is due to another cause. In addition to brushing and flushing with warm water, cautiously rotating the prosthesis a couple of times to dislodge any debris may help. If the leak persists the voice prosthesis should be replaced.
- Attempting to stop the leak by cleaning and brushing (see below)
- Stopping the leak by inserting an adequate plug (see below) into the prosthesis whenever consuming fluids or leaving it permanently and switching to alternate speaking method (e.g., esophageal speech, electrolarynx)
- Consuming viscous fluids that generally do not leak (i.e., yogurt, jelly, soup, oatmeal, etc) through or around the prosthesis (see below)
- Drinking small amount of fluid without strong effort while lying down, swallowing the liquid as if it is a food item, speaking a few words each time fluids are swallowed, can reduce or prevent the liquids from leaking into the trachea
It is important to stay well hydrated despite the leakage. Avoiding fluid losses in hot weather through perspiration by staying in an air-conditioned environment and ingesting liquids in a way that is less likely to leak are helpful. Drinks that contain caffeine increase urination and should be avoided.
Speaking a few words each time fluids are swallowed, leaning back, or lying down can reduce or even prevent the liquids to leak into the trachea.Viscous (thickened) fluids tend not to leak and consuming them can provide essential liquids despite the leak. Many food items that contain large amount of liquids are more viscous (i.e., jelly, soup, oat meal, toast dipped in milk, yogurt) and are therefore less likely to leak through the prosthesis. On the other hand coffee and carbonated drinks are more likely to leak. Fruits and vegetables (e.g., watermelon, apples, etc.) contain large amount of water. The way to find out what works is to cautiously try any of these.

Maintenance and prevention of leakage guidelines are:
- Before using the brush provided by the manufacturer, dip it in a cup of hot water and leave it there for a few seconds.
- Initially the mucus around the prosthesis should be gently cleaned using
tweezers preferably with rounded tips. Following that, the
manufacturer-provided brush should be inserted into the prosthesis (not too
deep) and rotated several times. The brush should be
thoroughly washed with warm water after each cleaning. The prosthesis is then
flushed twice with warm (not hot) water using the manufacturer’s provided bulb. .
- Take the brush out and rinse it with hot water and repeat the process 2-3 times until no material is brought out by the brush. Wait until the brush is not hot any more before brushing the prosthesis again. Be careful not to insert it beyond the voice prosthesis inner valve to avoid traumatizing the esophagus with excessive heat.
- Gently flush the voice prosthesis twice with water or saline using the bulb provided by the manufacturer using warm (not hot!) potable water. To avoid damage to the esophagus sip the water first to make sure that the water temperature is not too high. The flushing bulb should be introduced into the prosthesis opening while applying slight pressure to completely seal off the opening. The angle of inserting the end of the tip of the bulb varies between individuals. (The SLP can provide instructions how to choose the best angle.) Flushing the prosthesis should be done gently because using too much pressure can lead to splashing of water into the trachea. If flushing with water is problematic, the flushing can be done with air.
Dip the voice prosthesis brush in a small amount of mycostatin suspension, Chlorhexidine Gluconate (Pyridex) or vinegar and brush the inner voice prosthesis before going to sleep. (A homemade suspension can be made by dissolving a quarter of a mycostatin tablet in 3-5 cc water). This would leave some of the suspension inside the voice prosthesis. The unused suspension should be discarded. Do not place too much mycostatin, Chlorhexidine Gluconate (Pyridex), or vinegar in the prosthesis to prevent dripping into the trachea. Speaking a few words after placing the suspension will push it towards the inner part of the voice prosthesis
- Prevent formation of biofilm by yeast and bacteria (see next section)
Watch a video how to flush the voice prosthesis
- Reduce the consumption of sugars in food and drinks, brush your teeth well after consuming sugary food and/or drinks.
- Brush your teeth well after every meal and especially before going to sleep.
- Clean your dentures daily.
- Diabetic should maintain adequate blood sugar levels.
- Take antibiotics and corticosteroids only if they are needed.
- After using an oral suspension of an antifungal agent, wait for 30 minutes to let it work and then brush your teeth. This is because some of these suspensions contain sugar.
- Dip the voice prosthesis brush in a small amount of mycostatin suspension, Chlorhexidine Gluconate (Pyridex), or vinegar and brush the inner voice prosthesis before going to sleep. (A homemade suspension can be made by dissolving a quarter of a mycostatin tablet in 3-5 cc water). This would leave some of the suspension inside the voice prosthesis .The unused suspension should be discarded. Do not place too much mycostatin or vinegar in the prosthesis to prevent dripping into the trachea. Speaking a few words after placing the suspension will push it towards the inner part of the voice prosthesis.
- Consume probiotics by eating active-culture yogurt and/or a probiotic preparation.
- Gently brush the tongue if it is coated with yeast (white plaques).
- Replace the toothbrush after overcoming a yeast problem to prevent re colonizing with yeasts
- Keep the prosthesis brush clean
.jpg)

















No comments:
Post a Comment