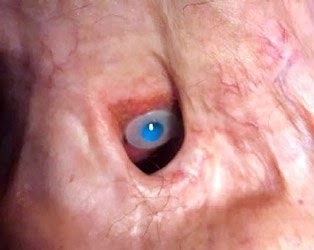
Laryngectomees, face many psychological,
social and personal challenges . Laryngectomees also experience social
isolation and loneliness (SIL) because of their difficulties in communication
and their post-surgical deformities. A study by Itzhak Brook MD from Georgetown University, published in European
Annals of Otorhinolaryngology, Head and Neck diseases; shed light on this issue
by evaluating the frequency of SIL in laryngectomees.
Members of Facebook laryngectomee support
groups were asked if they experience social SIL. Statistical analysis used:
'N-1' Chi squared test. A total of 379
individuals responded (208 males, 171 females). A total of 237 (62.6%) reported
SIL (117 males, 120 females). SIL was present in 117 males ( 56.2% of
males) and 120 of females ( 70.2 %
of females). Ninety four individuals (
61 males and 33 females) reported their method of speaking. SIL was reported in
voice prosthesis users in 17 (47%) males, and 12 (66%) females). It was
reported in electrolaryx users in 6 (24%) males, and 7 (43%) females. The
difference between males and females was not significant in either group.
However, the presence of SIL was significantly higher in all voice prosthesis
users compared to all electrolarynx users.) The higher frequency of SIL in
females compared to males may be due to their awareness of their anatomical
changes following laryngectomy.
SIL is common in cancer survivors,
contributing to poor outcomes and is associated with increased risk of
cardiovascular disease, hypertension, stress, decreased quality of life, poor
physical and mental health, and higher mortality. Loneliness was present in a
quarter of HNC patients.(5) Patients who
were younger, lived in deprived circumstances, had advanced disease and had been
treated with chemotherapy or radiotherapy reported greater levels of
loneliness. Loneliness was associated with a worse overall quality of life, and
worse physical and social-emotional function.
Despite the limitations of our analysis,
due to the use of a Facebook group that included various groups of
laryngectomees, and the lack of a validated standard test to analyze
loneliness, our data highlight the high frequency of SIL in laryngectomees. It
is hopeful that these findings would inspire further research and encourage
clinicians to recognize and treat SIL in laryngectomees. Early recognition and
interventions to relieve SIL are urgently needed.
link to the manuscript https://drive.google.com/file/d/1Vqqy1BBMYQa35a_J5bD7IT4Sx3r5JZ06/view?usp=sharing